Health issues rarely come in one. Your body is an interconnected system of cells, organs, tissues, hormones, and so on. If one thing goes wrong, chances are it will affect other areas of your body too. This is the thing with your thyroid.
Thyroid disease doesn’t just happen on its own. Your diet, lifestyle, and overall health all play a role. Increasing evidence suggests that your mast cells may also play a role in thyroid disease.
In this article, I want to discuss the connection between your thyroid and mast cells. You will learn what your thyroid is and what thyroid disease is. You will learn about hypothyroidism and its symptoms. I will go over the function of your mast cells and what mast cell activation syndrome is. You will learn about the connection between your thyroid and mast cell activation. I will discuss the connection between your thyroid, histamine, and your gut health. Finally, I will offer some natural strategies to improve your thyroid and mast cell health and overall well-being.
What Is Your Thyroid?
Your thyroid is a butterfly-shaped gland found right in front of your neck. It produces thyroid hormones that your body needs for energy. Your thyroid hormones support your digestion, breathing, heart rate, mood, weight, and other areas of your health (1, 2).
What Is Thyroid Disease
There are a variety of different thyroid diseases that can affect your thyroid health, including hyperthyroidism, hypothyroidism, goiter, thyroid nodules, thyroid cancer, and thyroiditis. For the purpose of this article, the thyroid disease I want to discuss is hypothyroidism, as it may be the most connected to mast cell activation issues.
What Is Hypothyroidism
Hypothyroidism is caused by an underactive thyroid. It means that your thyroid gland doesn’t make enough of some crucial thyroid hormones. Hashimoto’s disease is the most common form of hypothyroidism. It is an autoimmune condition where your immune system attacks your own thyroid. However, you can have non-autoimmune hypothyroid issues as well (3, 4, 5).
Causes of hypothyroidism:
- Nutrient deficiencies
- Environmental toxins
- Inflammatory diet
- Food sensitivities
- Gluten
- Chronic infections
- Heavy metals
- Mold
- Leaky gut syndrome
- Chronic stress
- Poor sleep
- Hormonal imbalances

Symptoms of hypothyroidism:
- Fatigue
- Sluggishness
- Sleepiness and sleep issues
- Increased sensitivity to cold
- Constipation
- Muscle weakness
- Muscles aches, stiffness, or tenderness
- Joint pain and stiffness
- Dry skin
- Brittle nails
- Hair loss
- Puffy face
- Depression
- Concentration issues
- Memory issues
- Brain fog
- Irregular periods
- Heavy periods
- Enlarged tongue
- Goiter (swelling of the thyroid)

Mast Cells and Histamine
Mast cell activation issues may be connected to your thyroid health. Before I get into this connection, I want to go over what are your mast cells, what histamine is, why you need them, and potential problems.
What Is Mast Cell Activation Syndrome
Your mast cells are essential for your immune and overall health. They are white blood cells that store histamine and other inflammatory mediators. They are located in your digestive tract, respiratory tract, urinary tract, skin, and blood.
When your body is attacked by an allergen, toxin, or other triggers, it will lead to mast cell activations. Your mast cells will cause an allergic response and release histamine along with other chemicals. This protective mechanism is essential for your immune health.
However, if your mast cells become dysregulated or overactive, it can turn into a serious issue. Mast cell activation syndrome (MCAS) means that your mast cells release too much histamine and other chemicals. This can lead to a variety of symptoms and affect your entire body. You may develop MCAS due to a variety of triggers, including mold, chemicals, toxins, heavy metals, allergens, medications, infections, viruses, food, and alcohol.
Symptoms of MCAS may include the following:
- Rashes
- Hives
- Itching
- Heart palpitations
- Low blood pressure
- Headaches
- Chest pain
- Weight changes, including rapid weight loss or weight gain
- Digestive trouble, including diarrhea, nausea, and vomiting
- Loss of appetite or low appetite
- Anxiety
- Fatigue
- Vision changes
- Weakness
- Dizziness
What Is Histamine Intolerance
Histamine gets a bad rap because of anti-histamine medications. The ‘anti’ part of anti-histamine, may make you believe that histamine is bad. It’s the opposite. Histamine is absolutely necessary for your health.
It is a chemical that supports your body in getting rid of allergens. It also supports your digestion by releasing hydrochloric acid to break down food and your brain health by serving as a chemical messenger. Too much of a good thing is rarely good, though.
If your body is releasing too much histamine and your body is unable to keep up and break down all the excess histamine, it will lead to histamine buildup. Histamine intolerance means that there is too much histamine in your body.
Under normal circumstances, your body sends enzymes to break down excess histamine and prevent build-up. If you have too much histamine or you don’t have enough of these enzymes, it won’t be able to break everything down, which can lead to histamine intolerance. Histamine intolerance can affect your entire body and lead to widespread symptoms.
Symptoms of histamine intolerance include the following:
- Itchy skin, eyes, ears, and nose
- Eczema or other types of dermatitis
- Hives
- Red eyes
- Facial swelling
- Crawling sensation on the skin or the scalp
- Tightness in the throat
- Difficulty regulating body temperature
- Sudden drop in blood pressure when standing up
- Low blood pressure
- Fast heart rate
- Heart palpitations
- Dizziness or vertigo
- Difficulty falling asleep or sleep issues
- Fatigue
- Confusion
- Brain fog
- Irritability
- Anxiety or panic attacks
- Congestion or runny nose
- Seasonal allergies
- Asthma
- Migraines and headaches
- Hair loss
- Acid reflux
- Diarrhea
- Abnormal menstrual cycle
- Premenstrual syndrome (PMS)
Mast Cell Activation Syndrome vs Histamine Intolerance
I believe that MCAS is the primary cause of histamine intolerance, but it may not be the cause for everyone. But considering the similarities between the symptoms of MCAS and histamine intolerance, you may feel confused.
Are these two conditions the same? No, they are not the same. Though symptoms of MCAS and histamine intolerance can be similar and are both caused by high levels of histamine, MCAS and histamine intolerance are not the same.
If your body has too much histamine and it can’t handle it, you may develop histamine intolerance. This usually happens due to a high-histamine diet. However, stress, poor sleep, environmental toxins, certain medications, and other factors may add to your histamine bucket as well. If your body has trouble breaking down the extra histamine, it will lead to histamine build-up and histamine intolerance.
While histamine intolerance simply means you have too much histamine in your body, you develop MCAS if your mast cells get triggered all the time. If you have MCAS, your mast cells get triggered by mold, allergens, or other triggers, they will release histamine and other chemicals into your body. Increased histamine release from mast cell activation can lead to too much histamine in your body. This can lead to a wide range of symptoms that are very similar to the symptoms of histamine intolerance.
As I mentioned before, MCAS is one of the primary causes of histamine intolerance. However, it is not the cause for everyone. You can have histamine intolerance without MCAS. You can also have MCAS without histamine intolerance. But you may have both MCAS and histamine intolerance. I see patients who have both conditions regularly (1, 2, 3).
If you have both conditions, your body will have increased difficulty breaking down the excess histamine. This can lead to widespread symptoms of MCAS and histamine intolerance. To figure out, whether you are dealing with symptoms of MCAS, histamine intolerance, or both. I recommend working with a functional medicine doctor who is well-versed in both conditions. (Tips: My team and I would love to help you with your diagnosis and treatment. Schedule your consultation here.)
To learn more about MCAS and histamine intolerance, I recommend reading my book, The 4-Phase Histamine Reset Plan: Getting to the Root of Migraines, Eczema, Vertigo, Allergies and More.
The Connection Between Thyroid Health and Mast Cells
Research, including a 2015 study published in Mediators of Inflammation, has found that mast cell activation may play a role in a variety of autoimmune conditions, including multiple sclerosis and rheumatoid arthritis (6). I have written an in-depth article about the connection between mast cells, histamine intolerance, multiple sclerosis, and other autoimmune issues. You can check out this article here.
It’s logical to assume that mast cell activation may also play a role in autoimmune thyroid issues, thyroid disease, and overall thyroid function. Though there is limited research on this connection, we have increased evidence on the topic. A 2016 review published in Archivos Venezolanos de Farmacología y Terapéutica has found that mast cell activation may be linked to autoimmune thyroid issues (7).
According to a 2019 review published in Frontiers in Cellular Neuroscience, thyroid antibodies can attach to the surface of your mast cells (8). When they bind to your mast cells, your mast cells may activate. It seems that if you have too many thyroid antibodies due to Hashimoto’s disease, it may lead to increased mast cell activation. This may increase your risk of MCAS and histamine intolerance (8).
Researchers also found that your mast cells may be able to synthesize and store your T3 hormones. This means that when your mast cells are activated, they not only release histamine and other chemicals, but they may also be affecting your thyroid hormone levels and thyroid function (8).
The review has also found that in hypothyroid conditions, an increased number of mast cells are common (8). A 2022 study published in Animals has also found an increase in mast cells, mast cell degranulation, and histamine in hypothyroidism (9). More mast cells can mean increased mast cell activation. This can lead to the increased release of histamine and other chemicals and consequent symptoms (8).
Researchers have also found that histamine can affect the release of TSH. Thus having an underactive thyroid may increase the chance of developing MCAS and histamine intolerance. Moreover, it seems that your mast cells may not only play an important part in autoimmune thyroid disease and thyroiditis but also in the follicular variants of papillary thyroid cancer (8).

The Connection Between Histamine and Thyroid Health
I also want to touch on how your gut health may play a role in the connection between mast cell issues, histamine intolerance, and thyroid disease. Just to recap, hypothyroidism may increase the number of mast cells. Since your mast cells are responsible for histamine production, more mast cells can lead to increased histamine release. This may lead to histamine intolerance and related issues.
In a healthy body, DAO enzymes can clean up excess histamine. If you have too much histamine, your body may not be able to handle it all. On top of that, if you have low DAO enzyme production, it will further decrease histamine breakdown. This will lead to increased histamine levels. The combination of high histamine levels, low DAO enzyme levels, and a high-histamine diet can set you up for small bacterial overgrowth (SIBO), gut health issues, and histamine intolerance.
A 2007 study published in the Journal of Clinical Endocrinology and Metabolism has found that people with hypothyroidism were significantly more likely to have SIBO compared to those without (10). According to a 2012 study published in the Medicinal Clinics of North America, SIBO may be present in over half of those with hypothyroid issues (11).
SIBO and gut microbiome imbalance may lead to decreased DAO production, increased mast cell activation, an increase in histamine-producing bacteria, and an increased risk of histamine intolerance. Increased mast cell activation may be negatively affecting your thyroid hormone levels and thyroid function (8). However, thyroid dysfunction itself may lead to further mast cell activation (9).
On the top of that, increased mast cell activation, histamine intolerance, and a high histamine diet may increase gut health issues. As you can see, this can quickly turn into a vicious cycle of thyroid dysfunction, mast cell activation, histamine intolerance, microbiome imbalance, and gut health issues. We need to address all these underlying and interconnected issues to improve your health.
To learn more about the connection between thyroid health and histamine, I recommend reading this article I’ve written. To learn more about the connection between your mast cells, histamine, and your gut, I recommend this article.

Recommendations for Thyroid and Mast Cell Health
Here are my recommendations to improve your thyroid and mast cell health naturally:
Get a Full Thyroid Panel
I recommend that you work with a functional medicine practitioner (hint: call our office and schedule your consultation here).
A full thyroid panel checks for:
- Thyroid-stimulating hormone (TSH)
- Thyroxine (Total & Free T4)
- Triiodothyronine (Free T3 & total T3)
- Reverse T3
- Thyroid peroxidase antibodies (TPO)
- Thyroglobulin antibodies
Why should you work with a functional medicine doctor instead of your regular healthcare provider? Most healthcare providers don’t use a complete thyroid panel and only look at your TSH. This doesn’t tell the full picture, and many issues may be missed.
If your thyroid doesn’t make enough T4 or T3, you have an underactive thyroid. This may indicate an autoimmune thyroid condition, Hashimoto’s disease. If your thyroid makes too much T4 or T3, you have an overactive thyroid condition. In most cases, this is an autoimmune condition, Graves disease. Most doctors only test for TSH instead of ordering a full thyroid panel, and they fail to diagnose thyroid issues. Your TSH may still be fine, while your T3 or T4 may be off already.
Functional medicine doctors also use a slightly different range. This helps us to detect preclinical thyroid issues before full-blown thyroid disease.
Checking your thyroid levels will not only help us with the proper diagnosis. Your test results can guide us in creating an individualized treatment plan. Regular testing can help us check your progress and adjust your treatment plan if needed.
Eat an Anti-Inflammatory, Thyroid-Friendly, and Low-Histamine Diet
I recommend following a low-histamine, anti-inflammatory, thyroid-friendly, nutrient-dense, whole-food diet. Remove inflammatory foods, including refined sugar, refined oils, canned and processed meat, artificial ingredients, junk food, and highly processed foods. Eat lots of greens, vegetables, herbs, spices, fruits, healthy fats, and organic meat.
Add lots of thyroid-supporting foods to your diet, including organic vegetables, wild-caught fish, olive oil, coconut oil, low-sugar fruits, such as cherries, cantaloupe, and berries, grass-fed and pasture-raised animal products, seaweed, herbs, and herbal tea. My book, The 30-Day Thyroid Reset Plan: Disarming the 7 Hidden Triggers That Are Keeping Your Sick, has some great recommendations for thyroid-friendly foods and meals.
However, if you are dealing with mast cell activation or histamine intolerance, along with thyroid issues, you have to follow a low-histamine diet. For example, fermented food and apple cider vinegar are great options for healthy individuals or those with thyroid issues without mast cell activation or histamine intolerance. However, if you have mast cell activation or histamine intolerance, you need to avoid fermented foods and apple cider vinegar as they are high in histamine.
Remove high-histamine foods and foods that can increase your histamine load. High-histamine foods that you should avoid include age cheese (e.g., goat cheese), citrus fruits, canned and cured meat (e.g., pepperoni, salami, bacon, lunch meat, hot dogs, and canned meat), dried fruits (e.g., apricots, dates, raisins, figs, and prunes), fermented foods (e.g., kefir, sauerkraut, soy sauce, and vinegar), fermented alcohol (e.g., beer, wine, and champagne), legumes (e.g., beans, lentils, soy, and peanut), certain nuts (e.g., cashew and walnuts), soured foods (e.g., buttermilk, sour milk, sour cream), smoked fish and certain types of fish (e.g., mackerel, mahi-mahi, anchovies, sardines, tuna, and fish sauce), certain vegetables (e.g., avocados, tomatoes, eggplant, and spinach), vinegar-containing foods (e.g., pickles and olives), and all overly processed foods because of the high histamine load from preservatives.
Avoid histamine-liberating foods that are low in histamine but trigger histamine release in your body, including alcohol, nuts, bananas, papaya, pineapple, strawberries, tomatoes, chocolates, wheat germ, cow’s milk, shellfish, and many artificial preservatives and dyes. Avoid DAO enzyme-blocking foods and drinks, such as alcohol, black tea, green tea, mate tea, and energy drinks.
Try new recipes. I recommend all the low-histamine recipes in The 4-Phase Histamine Reset Plan: Getting to the Root of Migraines, Eczema, Vertigo, Allergies and More and my recipe books, Fifty One Low Histamine Air Fryer Recipes and Low Histamine Cooking in Your Instant Pot.
Try Some Mast Cell-Stabilizing and Histamine-Reducing Foods and Supplements
You can boost the benefits of your anti-inflammatory, low-histamine diet by adding some foods that may help to reduce your levels of histamine and stabilize your mast cells. Quercetin helps to reduce histamine. Add quercetin-rich foods to your diet, such as grapes, apples, cranberries, black plums, cherries, black currants, chokeberries, blueberries, olive oil, cruciferous vegetables, kale, romaine lettuce, chicory greens, red leaf lettuce, cabbage, sprouts, asparagus, snap peas, peppers, and red onion. You may also try a quercetin supplement.
I also recommend adding foods that can help to stabilize your mast cells, including onion, peaches, nettle, apples, chamomile, moringa, watercress, Thai ginger, and fiber-rich foods. You may also try a DAO enzyme supplement to support histamine breakdown and HistoRelief.
HistoRelief is a synergistic blend of nutrients that provides natural support to balance your immune response. This blend features Tinofend®, a patented and clinically researched extract derived from the plant Tinospora cordifolia, which has a powerful ability to support immune regulation and immune response. As a result, it boosts your body’s ability to fight interstitial cystitis symptoms. It includes quercetin, nettle leaf, vitamin C, and bicarbonate salt to help inhibit histamine release, supports normal histamine metabolism, and improves immune health.
Reduce Your Histamine Load
Beyond a high-histamine diet, certain lifestyle choices may add to your histamine load as well. I recommend improving your lifestyle to reduce histamine intolerance. These lifestyle practices may also support your thyroid health, hormonal health, and overall health and wellness.
Reduce Your Stress Levels
Chronic stress can increase histamine intolerance, trigger mast cell activation, and impact your thyroid health. To reduce stress and improve sleep, I recommend practicing breathwork, meditation, positive affirmation, journaling, yoga, grounding, and time in nature for stress and anxiety reduction. Taking an Epsom salt bath is another great way to relax your muscles, calm your mind, and detoxify your body.
Get Enough Sleep Sleep
Inadequate and poor sleep is another major root cause behind histamine intolerance, MCAS, and thyroid issues. Make sure to sleep at least 7 to 9 hours a night. I recommend that you reduce your stress levels throughout the day but especially in the evening time to support sleep. Take a bath, read a good book, listen to some music, journal, try coloring, and spend time with your family. Avoid sugar, alcohol, and heavy food in the evening. I recommend investing in a supportive mattress, comfortable and supportive pillows and blankets, and quality, organic cotton sheets.
Move Your Body
A lack of movement may also increase the risk of histamine intolerance and thyroid problems.. Moving your body is a great way to reduce stress, improve detoxification, support hormonal health, support lymphatic flow, boost your mood, and support your overall health. Stay active throughout the day by taking a stroll in the park, stretching regularly, dancing to your favorite songs, playing with your kids or pets, and finding creative ways to incorporate movement. A standing desk or treadmill desk may be a great idea. Exercise at least 20 to 30 minutes five days a week and move your body regularly. I recommend getting 10 to 15K steps in a day if you can. Add resistance and strength training to your routine.
Remove Toxins
Toxin overload can increase chronic inflammation, mast cell activation, histamine release, histamine intolerance and thyroid dysfunction. I recommend reducing your exposure to environmental toxins. Use a high-quality air filtration system for better indoor air. Drink purified water to avoid toxins from your tap water. Avoid conventional cleaning, hygiene, body, and beauty products as they are loaded with chemicals. Choose natural, organic, and homemade options instead. Reduce the use of plastic and avoid BPA completely. Choose glass, bamboo, wood, organic cotton, silicon, and other natural alternatives instead of plastic. Avoid overly processed food products that can contain artificial ingredients. Choose organic food whenever possible.
Reduce Your Mast Cell Triggers
There are a number of triggers that can lead to mast cell activation and related histamine release and symptoms. Mast cell triggers tend to come from your environment. Common triggers of MCAS include mold, allergens, chemicals, toxins, heavy metals, and viruses.
Improve Your Gut Health
As you’ve learned your gut health and gut microbiome imbalance may be closely connected to thyroid disease, mast cell activation, and histamine intolerance. We have to address all areas of the puzzle. Improving your gut health is critical for improving your symptoms and regaining your health. Along with a gut-friendly anti-inflammatory diet, I recommend that you take a high-quality probiotics supplement to support your gut microbiome balance. For further gut-supporting supplements and a specific gut-health protocol, I recommend working with a functional medicine practitioner, like us.
Try Thyroid-Supporting Nutrients
You may also try to add some thyroid-supporting nutrients to your regimen:
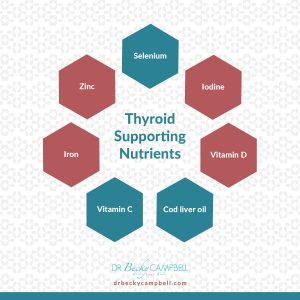
Selenium
Selenium is a great nutrient for thyroid function. It may help to protect your thyroid from too much iodine exposure. It may also be important for the conversion of T4 into T3. Selenium may also help to reduce inflammatory activity, which may reduce the risk or symptoms of autoimmune thyroid disease (12). The best part of selenium is that you don’t even need to supplement. Food form is usually better. Only two Brazil nuts a day should cover your selenium needs. Fish and organ meat are also great sources.
Iodine
Iodine is absolutely critical for thyroid hormone synthesis (13). Being a woman at child-bearing age, pregnancy, and being vegan may increase your risk of deficiencies. Children are also at a higher risk. Seaweed, fish, eggs, and beef liver may be good sources of iodine. Iodized table salt has also become popular in the past decades to reduce deficiencies.
However, too much iodine can also be a problem, especially if there is a selenium deficiency present too. It’s important that you only supplement with iodine if you have an actual deficiency and use a thyroid-specific supplement with a proper iodine-selenium balance.
I recommend that you start with your diet first instead of reaching for expensive supplements. I recommend that you work with a functional medicine practitioner and get some blood testing done before any supplementation. We can help you spot your actual nutrient deficiencies and specific needs. We can figure out what you may benefit from beyond your diet. This will prevent you from spending money on supplements that you may not need and only using the ones that actually support your health and well-being.
Cod Liver Oil and Vitamin D
Vitamin D is essential for your immune system, bone health, muscle health, brain and mental health, and other areas of your health (14). Vitamin D deficiency may also increase your risk of hypothyroidism (15). Sunshine is the best way to boost your vitamin D levels. However, with our indoor lifestyle, cold climates, and fear of harm from UV damage, most of us don’t meet our needs from sunshine alone.
Cod liver oil is a fantastic source of vitamin D, A, and E, and omega-3 EPA and DHA. These nutrients may all help to support your immune health and reduce inflammation. For some people, cod liver oil supplementation is enough. Others may require additional vitamin D supplementation.
Vitamin C
Vitamin C is a powerful antioxidant that may also help to protect your body (16). Lemon, lime, oranges, grapefruit, tangerines, and other citrus are great sources of vitamin C. However, citrus may be triggering histamine intolerance. Some people notice that they can tolerate some citrus fruits and others they cannot. That is why they are on my maybe list. I encourage you to see how you respond. I could always tolerate lime, but couldn’t tolerate lemon for a while. Other great and low-histamine sources of vitamin C include kiwi, bell pepper, broccoli, Brussels sprouts, cabbage, and cauliflower.
Curcumin and Resveratrol
Curcumin is the active compound of the spice turmeric. Resveratrol is a polyphenol found in the skin of grapes, red wine, berries, and pistachios. They offer antioxidant, immune-supporting, and anti-inflammatory benefits that may help to reduce the risk and symptoms of autoimmunity (17, 18). Thus they may help with autoimmune thyroid issues (19, 20). You may benefit from consuming food rich in curcumin and resveratrol. You may also benefit from supplementation.
Iron
Iron deficiency may increase the risk of issues with thyroid hormone production It may reduce thyroid peroxidase activity in the thyroid. However, too much iron can also become an issue. Too much iron may increase the risk of thyroid issues and iron toxicity (21).
Don’t take iron supplements, unless you actually need it. Consume iron-rich foods, including beef, liver, oysters, clams, and venison. Get your iron levels tested. If your doctor finds iron deficiency, you may benefit from iron supplementation, usually only short-term.
Zinc
Zinc is a powerful mineral that is essential for your immune health and hormonal balance. It plays a role in the conversion of T4 to T3 and supports normal T4 and T3 levels (22). Food rich in zinc include oysters, red meat, poultry, and lobsters. Broccoli, spinach, mushrooms, kale, and garlic also contain plenty of zinc.

Check Out the Health Babes’ Guide to Balancing Your Hormones
To learn more about your hormones and learn how to improve your hormonal health naturally, I recommend our book (co-authored by Dr. Krystal Hohn and myself) The Health Babes’ Guide to Balancing Your Hormones: A Detailed Plan with Recipes to Support Mood, Energy Levels, Libido, and More. This book is not only full of information but with an easy-to-follow plan and easy-to-make, delicious hormone-friendly recipes.
Final Thoughts
Your thyroid health and your mast cells may be connected. Underlying mast cell activation issues are not uncommon in thyroid disease. If you are dealing with thyroid health issues, I recommend looking into potential underlying mast cells and histamine-related issues and addressing them as well.
If you are dealing with symptoms of MCAS or histamine intolerance, I invite you to schedule a consultation with us. We can help identify the root cause of your condition and recommend a personalized treatment plan to repair your body and regain your health and well-being. Schedule your consultation here. You can also get started on your own with my Histamine Online Program.
Sources I:
- Thyroid test National Institute of Health. National Institute of Diabates and Digestive and Kidney Disease link Here
- Beynon ME, Pinneri K. An Overview of the Thyroid Gland and Thyroid-Related Deaths for the Forensic Pathologist. Acad Forensic Pathol. 2016 Jun;6(2):217-236. doi: 10.23907/2016.024. Epub 2016 Jun 1. PMID: 31239894
- Fasano, A. (2012). Leaky gut and autoimmune diseases. Clinical Reviews in Allergy and Immunology, 42(1), 71–78. PMID: 22109896
- Mu, Q., Kirby, J., Reilly, C. M., & Luo, X. M. (2017). Leaky gut as a danger signal for autoimmune diseases. Frontiers in Immunology. PMID: 28588585
- Pollard, K. M., Hultman, P., & Kono, D. H. (2010). Toxicology of autoimmune diseases. Chemical Research in Toxicology. PMID: 20078109
- Xu Y, Chen G. Mast cell and autoimmune diseases. Mediators Inflamm. 2015;2015:246126. doi: 10.1155/2015/246126. Epub 2015 Apr 5. PMID: 25944979
- Rojas, J. Mast cell activation disease associated with autoimmune thyroid disease: case report and review of literature Archivos Venezolanos de Farmacologica y Terapeutica 2016
- Landucci E, Laurino A, Cinci L, Gencarelli M, Raimondi L. Thyroid Hormone, Thyroid Hormone Metabolites and Mast Cells: A Less Explored Issue. Front Cell Neurosci. 2019 Mar 29;13:79. doi: 10.3389/fncel.2019.00079. PMID: 30983971
- Baccari. Animals. 2022. Mast Cell Population and Histamine Content in Hypothyroid Rat Tissues.
- Lauritano, E.C., Bilotta, A.L., Gabrielli, M., Scarpellini, E., Lupascu, A., Laginestra, A., et al. Association between hypothyroidism and small intestinal bacterial overgrowth. J Clin Endocrinol Metab. 2007;92:4180–4. Link here
- Almandoz, J.P., Gharib, H. Hypothyroidism: Etiology, diagnosis, and management. Med Clin North Am. 2012;96:203–21. Link Here
Sources II:
- Ventura M, Melo M, Carrilho F. Selenium and Thyroid Disease: From Pathophysiology to Treatment. Int J Endocrinol. 2017;2017:1297658. doi: 10.1155/2017/1297658. Epub 2017 Jan 31. PMID: 28255299
- Chung HR. Iodine and thyroid function. Ann Pediatr Endocrinol Metab. 2014 Mar;19(1):8-12. doi: 10.6065/apem.2014.19.1.8. Epub 2014 Mar 31. PMID: 24926457
- Aranow C. Vitamin D and the immune system. J Investig Med. 2011 Aug;59(6):881-6. doi: 10.2310/JIM.0b013e31821b8755. PMID: 21527855
- Mackawy AM, Al-Ayed BM, Al-Rashidi BM. Vitamin d deficiency and its association with thyroid disease. Int J Health Sci (Qassim). 2013 Nov;7(3):267-75. doi: 10.12816/0006054. PMID: 24533019
- Carr AC, Maggini S. Vitamin C and Immune Function. Nutrients. 2017 Nov 3;9(11):1211. doi: 10.3390/nu9111211. PMID: 29099763
- Hewlings SJ, Kalman DS. Curcumin: A Review of Its Effects on Human Health. Foods. 2017 Oct 22;6(10):92. doi: 10.3390/foods6100092. PMID: 29065496
- Meng T, Xiao D, Muhammed A, Deng J, Chen L, He J. Anti-Inflammatory Action and Mechanisms of Resveratrol. Molecules. 2021 Jan 5;26(1):229. doi: 10.3390/molecules26010229. PMID: 33466247
- Abdelaleem MM, El-Tahawy NFG, Abozaid SMM, Abdel-Hakim SA. Possible protective effect of curcumin on the thyroid gland changes induced by sodium fluoride in albino rats: light and electron microscopic study. Endocr Regul. 2018 Apr 1;52(2):59-68. doi: 10.2478/enr-2018-0007. PMID: 29715188
- Duntas LH. Resveratrol and its impact on aging and thyroid function. J Endocrinol Invest. 2011 Nov;34(10):788-92. doi: 10.3275/7926. Epub 2011 Sep 23. PMID: 21946130
- Soliman AT, De Sanctis V, Yassin M, Wagdy M, Soliman N. Chronic anemia and thyroid function. Acta Biomed. 2017 Apr 28;88(1):119-127. doi: 10.23750/abm.v88i1.6048. PMID: 28467346
- Maxwell C, Volpe SL. Effect of zinc supplementation on thyroid hormone function. A case study of two college females. Ann Nutr Metab. 2007;51(2):188-94. doi: 10.1159/000103324. Epub 2007 May 30. PMID: 17541266
You Might Also Like
7 Natural Ways to Clear Histamine From the Body
If you suffer from symptoms of histamine intolerance like hives, headaches, or GI symptoms, one of the best things you…
What is PCOS and What Can You Do About It?
PCOS stands for polycystic ovarian syndrome and something that I see in my practice all the time. It is also one of the…
Ready to Improve Your Health?
Get Started on Your Journey to Wellness





