You went out to eat the other night and had your favorite dinner: tuna tartare paired with sautéed spinach and a glass of your absolute favorite red wine. Overnight, you developed a huge rash that covers your entire chest, and today, you’ve noticed the start of several open sores, or at least a rash, on the back of both sides of your neck. What is the deal?! Come to think of it, the last time you came to this same restaurant, you had seafood and wine, and the next day, you remember a similar reaction. What does this mean? Today we are going to cover the causes, symptoms, and complications of eczema, it’s potential relationship to histamine intolerance, and what you can do to manage your eczema symptoms long-term.
What is eczema?
Eczema, also referred to as atopic dermatitis (AD), is a chronic skin condition that usually starts in infancy that is characterized by exacerbation and remission of episodes of skin lesions. Other symptoms of eczema include:
- dry skin
- itching, especially at night
- red to brownish-gray skin patches
- small raises bumps which may leak initially or when scratched and then form a crust
- thick, cracked, or scaly skin patches
- raw and/or sensitive skin.
Usually (not always) atopic dermatitis symptoms begin before age 5, but may continue up through adulthood. Unlike psoriasis, AD symptoms are not present all the time. Remission could even last for several years in some cases. The biggest issue with eczema is an increased risk of skin infection (look for white-yellow discharge, fever) and inability to get a good night’s sleep. If you suspect an infection or are so uncomfortable you can’t get a good night’s rest, follow up with a physician you trust (1).
Why do people have eczema?
The presence of eczema in some people can be traced back to a gene variation that affects your skin’s ability to provide protection from bacteria, irritants, and allergens. Without this inherent protection, your skin will be more affected by things you come into contact with in your environment. The primary risk factor for developing eczema is a family history of eczema, allergies, hay fever, or asthma (which can all be caused by histamine intolerance just FYI). However, as we will further discuss below, food sensitivities and a “leaky gut” can also play a huge role in whether you will have a flare-up or not (2).
Eczema triggers
If you know you have AD, you have to figure out what your triggers are. While they may be different for everyone, here is a list of commonly identified triggers that will give you a place to start.
- Chemical Irritants: these are products that you use daily, including dish soaps, body wash, shampoos, laundry detergents, or other cleaning products. Similarly, some people can have a reaction to their jewelry or clothing, including both the fabric of the clothing as well as any irritation from a tag rubbing on your skin.
- Environmental Irritants: when you have a hyperactive immune system, items like pet dander (cats > dogs), mold, dust mites, pollen, dandruff can cause your immune system to overreact, leading to a skin reaction.
- Extreme temperatures: weather changes as well as temperatures greater than 80 degrees F or less than 30 degrees F as well as changes in humidity can cause an immune reaction and can trigger eczema symptoms for many people.
- Stress: Symptoms of eczema can become more pronounced if someone is under mental and/or emotional stress.
- Food sensitivities: There are many types of food allergens and sensitivities that can trigger an eczema flare-up. The most common include gluten, dairy, corn, eggs, chocolate, nuts, and soy. This will be further discussed below under “SIBO and Food Sensitivities.”
- Hormone levels: Changes in your hormones levels can also aggravate eczema symptoms. For example, some women notice an increase in their eczema around the timing of their menstrual cycle.
- Microbial overgrowth: An unhealthy gut and the presence of bacteria like E.coli and staph can increase eczema symptoms. This will be further discussed in “Eczema, Histamine, and Gut Health” (2).

Eczema and Gut Health
As we know, the purpose of our skin is to act as one of the first barriers to the outside from physical, chemical, and microbial stressors. Irritation of the gut, caused by microbial overgrowth, combined with the genetic variation discussed above can decrease the effectiveness of your skin’s barrier. This will diminish the number of antibacterial proteins produced in the skin and can lead to hyper-inflammation and potential infections, both of which are hallmark signs of eczema/AD (2,3).
Similarly, the gut flora can influence what the skin is generating for protection from the environment, including fatty acids and oil (sebum) production. A change in these skin components related to a high microbe count or increased inflammation from food sensitivities can result in more inflammation and infection of the skin cells in the area, causing the development of acne, redness, and eczema (2).
Eczema and Histamines
When the skin is irritated, it produces a message transmitter called substance P. This chemical will cause the release of histamine from mast cells in the area, which will result in an inflammatory response. People with poor bacterial balance in their gut have increased substance P production, which will result in more histamine release and a hyper-inflammatory response (2).
There is some research to suggest that oral intake of probiotics will reduce skin inflammation, reinforce the skin barrier, and decrease skin sensitivity more than a topical medication to reduce the symptoms (2,4). That being said, not all probiotics work well with those with histamine intolerance. I like probiota histaminX from seeking health. Treating the reason behind the eczema will be more effective than just treating the symptoms.
Small Intestinal Bacterial Overgrowth (SIBO) and Food Sensitivities
An altered gut flora and an increase in intestinal permeability can cause an exaggerated immune response to specific foods. Research indicates that people dealing with eczema and other chronic skin conditions are irritated by certain foods (5,6).
The most commonly noted food sensitivities are wheat, gluten, dairy, soy, corn, eggs, nuts, chocolate, and sugar (2).
Natural Solutions for Eczema and Histamine Intolerance
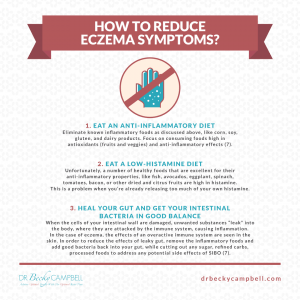
I recommend the following natural strategies for eczema and histamine intolerance:
Follow an Anti-Inflammatory and Low-Histamine Diet
Following an anti-inflammatory, antioxidant-rich, and nutrient-dense diet is important for your skin health. Reducing inflammation through an anti-inflammatory diet can reduce skin inflammation and skin symptoms. Following a low-histamine diet can help you reduce histamine intolerance and lower the risk of histamine-related eczema and skin issues.
Remove inflammatory foods, including refined sugar, refined oils, canned and processed meat, artificial ingredients, junk food, and highly processed foods. Avoid high-histamine foods, such as fermented food (e.g., sauerkraut, kimchi, fermented vegetables, kombucha, etc.), aged food (e.g., aged cheese, processed meat, canned fish, etc.), over-ripe fruits and vegetables, leftovers, and foods that are naturally high in histamine (e.g., avocadoes, eggplant, spinach, dried fruits, etc.). Avoid foods that may trigger histamine releases, such as tomatoes, most citrus, bananas, most nuts, and dairy. Avoid foods that may block the DAO enzyme, including black tea, green tea, alcohol, and energy drinks.
Eat a nutrient-dense, anti-inflammatory, and low-histamine diet rich in greens, vegetables, herbs, spices, fruits, healthy fats, and organic meat. Low-histamine foods include most fresh leafy greens and vegetables, non-citrus fruits, such as apples, pear, papaya, and grapes, fresh grass-fed meat, pasture-raised poultry and eggs, and wild-caught fish, olives, extra-virgin olive oil, ghee, coconut oil, leafy herbs, and herbal tea. My book, The 4-Phase Histamine Reset Plan includes an extensive list of foods that you can eat and should avoid on a low-histamine diet.
If you are new to a low-histamine diet, remember to have fun experimenting with new foods and recipes. I promise low-histamine meals can be delicious. I recommend all the low-histamine recipes in The 4-Phase Histamine Reset Plan and my new recipe book, Fifty One Low Histamine Air Fryer Recipes. They are all simple, easy to make, low-histamine, gluten-free, Paleo-friendly, and super healthy. Not to mention how delicious they are — your family will love them too.
Avoid Irritants and Lower Your Histamine Bucket
Avoid allergens and irritants that may trigger your eczema. Remove conventional cleaning, hygiene, and beauty products, and use organic, natural, and homemade alternatives instead. Avoid fabric that may irritate your skin. If you are allergic to any metals, avoid wearing them, and choose surgical steel, silver, or gold instead. Make sure that your house is free from mold and use a high-quality air filtration system to reduce toxins in your indoor air. Beyond reducing exposure to environmental toxins, lower your histamine bucket by reducing stress, getting restful sleep, and moving your body regularly.
Support Your Gut
Your gut health affects your entire body. Gut flora imbalance can trigger both histamine intolerance and eczema. Supporting your gut health is critical for your recovery. Along with a gut-friendly, low-histamine, anti-inflammatory diet, I recommend that you take a high-quality probiotics supplement, such as ProBiota HistaminX probiotics, to support your gut microbiome balance.
Try Some Supplements
I recommend HistoRelief. It is a synergistic blend of nutrients that provides natural support to balance your immune response. This blend features Tinofend®, a patented and clinically researched extract derived from the plant Tinospora cordifolia, which has a powerful ability to support immune regulation and immune response. As a result, it boosts your body’s ability to fight eczema symptoms. It includes quercetin, nettle leaf, vitamin C, and bicarbonate salt to help inhibit histamine release, support normal histamine metabolism, and improve immune health.
Protect Your Skin and Use Natural Skincare
I have already covered that avoiding your triggers, such as chemicals, fabrics, and metals that may cause a problem, is important. There are others ways to protect your skin, though. If you live in a cold climate and are sensitive to cold weather, make sure to protect your skin with warm gloves and layers in sensitive areas.
Though proper hygiene, such as hand-washing, are critical for keeping infections, including skin infections, away, washing your hands too much can cause dry skin and trigger skin issues. You may want to use gloves when washing dishes. As I explained earlier, avoid conventional cleaning and personal hygiene products, such as chemical-filled soap, dish soap, body wash, or shampoo. Choose organic, natural, and homemade alternatives instead. You may learn more about my skincare routine in this article.
Though addressing underlying problems behind your eczema and dermatitis is key to recovery, it can take several months to improve those issues. In the meantime, you can reduce your symptoms naturally. Moisturizing and other topicals may help to reduce symptoms during flares. However, conventional topicals are filled with chemicals and can cause side effects and further skin issues. Instead, I recommend natural alternatives. The following options may help soothe your symptoms until you completely address your underlying problems. Coconut oil, colloidal oatmeal lotion and baths, aloe vera, and honey may all be great for eczema (7, 8, 9).
Final Thoughts
Eczema is an uncomfortable skin conditions characterized by inflamed, itchy, dry, scaly, and flaky skin. Histamine intolerance is one of the most common underlying issues behind eczema. Improving histamine intolerance may also help to improve your eczema symptoms. I recommend following the strategies outlined in this article to improve your symptoms and overall health.
If you are dealing with symptoms of histamine intolerance and eczema, I invite you to schedule a consultation with us. We can help identify the root cause of your condition and recommend a personalized treatment plan to repair your body and regain your health and well-being. Schedule your consultation here. I also recommend that you check out my Histamine Online Program.
Sources
- https://www.mayoclinic.org/diseases-conditions/atopic-dermatitis-eczema/symptoms-causes/syc-20353273.
- https://drjockers.com/beat-eczema-acne-psoriasis/.
- Slominski A. A nervous breakdown in the skin: stress and the epidermal barrier. The Journal of Clinical Investigation. 2007;117(11):3166-3169.
- Benyacoub J, Bosco N, Blanchard C, Demont A, Philippe D, Castiel-Higounenc I, Guéniche A. Immune modulation property of Lactobacillus paracasei NCC2461 (ST11) strain and impact on skin defenses. Benef Microbes. 2014 Jun 1;5(2):129-36.
- Eczema: Can eliminating particular foods help? Link Here.
- Atopic Dermatitis and Disease Severity Are the Main Risk Factors for Food Sensitization in Exclusively Breastfed Infants Link Here.
- Reynertson KA. JJD. 2015. Link Here
- Zagórska-Dziok M, Furman-Toczek D, Dudra-Jastrzębska M, Zygo K, Stanisławek A, Kapka-Skrzypczak L. Evaluation of clinical effectiveness of Aloe vera – a review. J Pre Clin Clin Res. 2017;11(1):86-93. Link Here
- Samarghandian S, Farkhondeh T, Samini F. Honey and Health: A Review of Recent Clinical Research. Pharmacognosy Res. 2017 Apr-Jun;9(2):121-127. doi: 10.4103/0974-8490.204647. PMID: 28539734
You Might Also Like
How the Body Detoxes Mycotoxins and Why It’s Harder for Some
Understanding mycotoxins metabolism, detox blocks, and how to move forward. You’re doing all the right things, but…
How to Manage Hashimoto’s Thyroiditis: Simple Steps for Lasting Relief
Natural Ways to Improve Thyroid Function, Boost Energy, and Regain Your Health Living with Hashimoto’s Thyroiditis can…
Ready to Improve Your Health?
Get Started on Your Journey to Wellness






